|
|
|
Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. and payment systems strengthen the PHC orientation of health systems by:
Promoting PHC as the first point of contact
Increasing the accessibility of priority interventions to the entire population
Supporting the integration of individual services and public health
Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. and provider payment systems refer to the transfer of pooled funds on behalf of the population to primary health care (PHC) providers to deliver health services. Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. means actively linking the allocation of funds to providers with information on their performance and the health needs of the population that they serve.
Payment systems that include a diverse mix of aligned methods encourage providers to promote access to necessary health services for patients, incentivize quality of care, and improve equity while promoting the efficient use of resources, and when appropriate, cost-containment.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Before taking action, countries should first determine whether purchasing & payment systems are an appropriate area of focus and where to target improvement efforts. Read on to learn how to use country data to:
- Make informed decisions about where to spend time and resources
- Track progress and communicate these updates to constituents or funders
- Gain new insights into long-standing trends or surprising gaps
- Countries can measure their performance using the Vital Signs Profile (VSP). The VSP is a first-of-its-kind tool that helps stakeholders quickly diagnose the main strengths and weaknesses of primary health care in their country in a rigorous, standardized way. The second-generation VSP measures the essential elements of PHC across three main pillars: Capacity, Performance, and Impact. Purchasing & payment systems are measured in the Financing domain of the VSP (Capacity Pillar).
If a country does not have a VSP, it can begin to focus improvement efforts using the subsections below, which address:
- Key indications
-
If your country does not have a VSP, the indications below may help you to start to identify whether purchasing & payment systems are a relevant area for improvement:
- Out-of-pocket expenditure: if effective purchasing and payment systems are not in place, it is likely there is a high out-of-pocket expenditure for primary care services that patients will experience, often creating financial hardship or preventing patients from accessing care altogether
- Misalignment of incentives for provider payment methods: if incentives for providers are not taken into consideration and/or discussed, this can lead to misalignment of the types of incentives in place leading to more ineffective purchasing and payment systems and diminishing the effect that provider incentives can have on the quality, efficiency and equity of care.
- Key outcomes and impact
-
Countries that improve purchasing & payment systems may achieve the following benefits or outcomes:
- First contact accessibility: strategic purchasing and payment systems help to put primary care services at the centre of the health system by increasing the accessibility of priority interventions and reinforcing a PHC-centric approach
- Protecting patients from financial risk: when it comes to PHC, and UHC in general, protecting people from financial risk and hardship, and preventing the act of paying for services from being something that adversely affects their quality of life are both key goals that can be achieved through strategic purchasing and payment systems
- Improve quality, equity, and efficiency of PHC: efficient and effective health financing, which includes strategic purchasing and payment systems, provides access to quality PHC even for marginalized populations who initially do not have the capacity to access services
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Explore this section for a curated list of actions that countries can take to improve purchasing & payment systems in their context, which embark on:
- Explaining why the action is important for purchasing & payment systems
- Describing activities/ interventions countries can implement to improve
- Describing the key drivers in the health system that should be improved to maximize the success/impact of actions
- Curating relevant case studies, tools, &/or resources that showcase what other countries around the world are doing to improve as well as select tools and resources.
Key actions:
-
Paying for services can often lead to great financial hardship for millions all over the world when things like out-of-pocket expenditure are extremely high, leaving people in situations that adversely affect their quality of life. A goal of strong PHC and UHC is to protect people from financial risk and hardship when they seek out health care services. Effective, or rather strategic, purchasing and payment systems work to ensure that this is present and ultimately prevent any negative financial impact that may occur when accessing care. 28
Key activities
National &/or sub-national levels
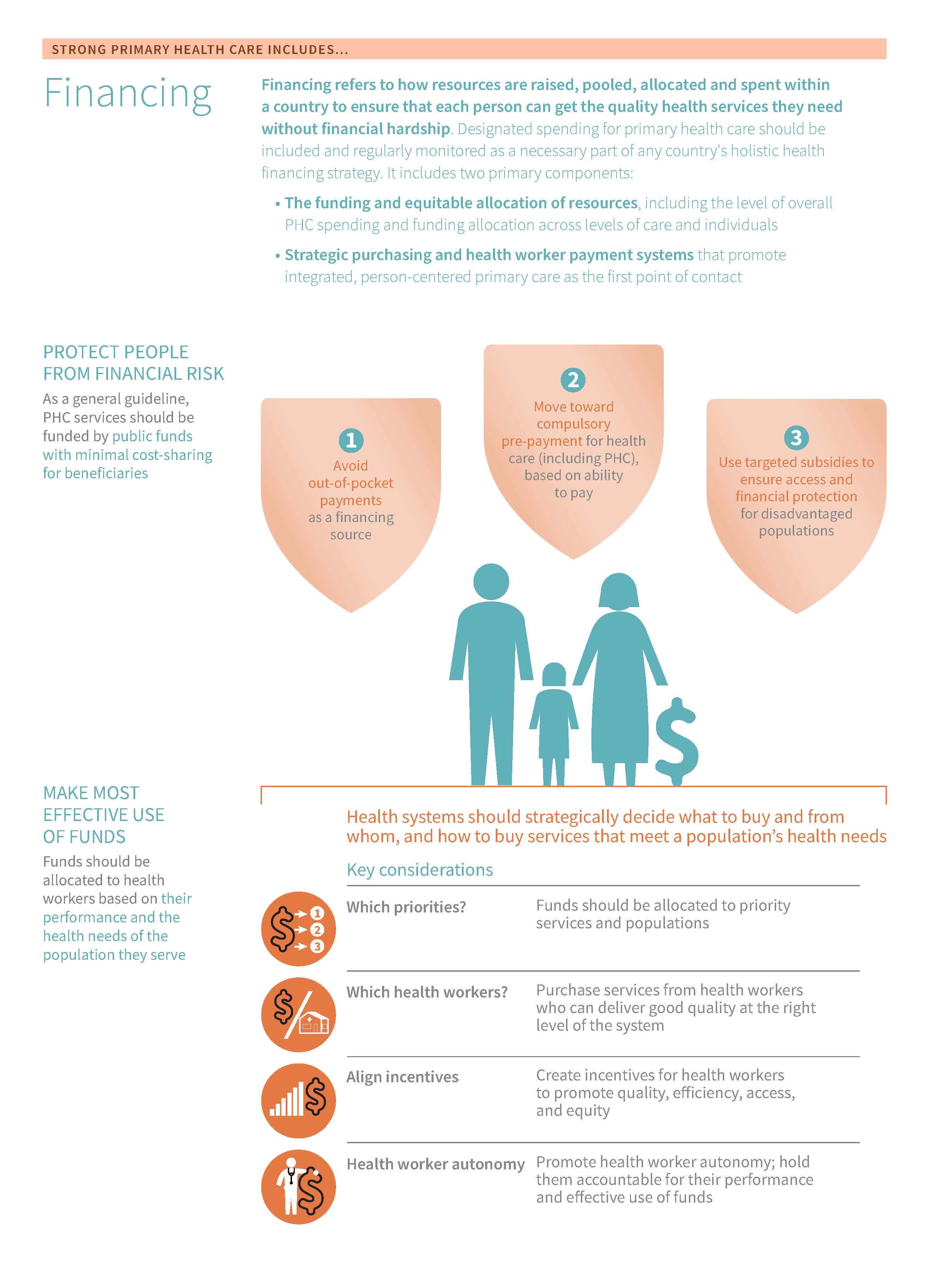
- Minimize out-of-pocket payments as a source of financing: Policymakers should avoid relying on out-of-pocket payments to fund PHC. PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. should be funded by public funds with minimal cost-sharing for beneficiaries. To ensure that a person’s ability to pay does not determine their access to health care, health policymakers can reduce cost-sharing to finance health care (or rely on small fixed cost-sharing payment amounts rather than proportional cost-sharing); services can be offered free of charge to defined population groups with certain easily observable socio-demographic criteria (such as age or poverty status), or high-priority health services such as those at the primary care level can be provided free of charge. 1229
- Move towards compulsory prepayment for health care, based on ability to pay: should rely on compulsory payments, such as taxes or national health insurance contributions and these funds should be pooled to purchase health care. These contributions should also be based on a household's ability to pay, as it works to promote the UHC objective of fairness in financing. Raising revenue through progressive taxation or based on a percentage of shared income works to promote fair financing. Additionally, Moving toward compulsory payments enhances redistributive capacity and also allows for cross-subsidization across the population. 29
- Move towards for health care: There are various ways to pool funds for health care and address fragmentation which both help to spread out the financial risk of paying for health services. The desirable attributes of a pool are large size in terms of the number of people covered by the pool and the diversity of health risks within the pool. 820 At best, the country’s arrangement avoids fragmentation, which may be characterized by multiple segmented pools, health insurance coverage for the formal sector employees only, or multiple territorially overlapping pools. 30
District &/or facility level
- Targeted financial protection schemes: targeting approaches can include means testing (identifying eligible households by measuring their income, housing characteristics, or assets), geographic targeting (identifying eligible households based on location, such as a malaria-endemic region or highly mountainous area with difficult access to health services), and characteristic targeting (identifying eligibility based on characteristics such as ethnicity, age, gender, education, pregnancy or disease). 31 Targeting can be used to exempt vulnerable groups from user fees at the point of care; this is more feasible if the eligibility criteria are based on easily observable characteristics, such as age, sex, or pregnancy status, since health facility personnel may not be best positioned to identify who meets other targeting criteria. The identification process could also be handled outside of the facility and individuals can be given an exemption card. Alternatively, eligible groups can be enrolled in a health coverage scheme and have their “contributions” paid on their behalf by the government. 32 Eligible individuals should be pre-identified through other existing mechanisms to minimize administrative costs. 9
- Protect population groups at risk of financial hardship: Countries can use household expenditure surveys, which measure household socioeconomic status and levels of health care spending, to identify which income level groups are spending a burdensome fraction of their income on health care costs. Understanding who is most at risk of catastrophic expenditures (e.g., elderly people, poor and vulnerable groups?), and for what kinds of health care costs (e.g. paying for medicines, hospital care, chronic disease care?), can help health policymakers develop strategies for improving . Household surveys can also indicate whether households forego care seeking for PHC due to financial barriers.
Related elements
- Policy & leadership
- Adjustment to population health needs
- Funding & allocation of resources
- Population health management
- Management of services
Relevant tools & resources
- P4H, 2022: P4H Social Health Protection Network
- SP4PHC, 2022: Strengthening Strategic Purchasing for Primary Care - Financial Protection
- WHO, 2018: Voluntary Health Insurance: Potentials and limits in moving towards UHC
- WHO, 2017: Free Health Care Policies: Opportunities and Risks for Moving Towards UHC
- Kutzin et al., 2016: Alternative Financing Strategies for UHC
- WHO, 2016: Health Financing Country Diagnostic: A Foundation for National Strategy Development
-
The way a country purchases its health care can have an immense impact on how the health system performs. A well-aligned mix of provider payment methods can encourage providers to promote access to necessary health services for patients, incentivize quality of care, and improve equity while promoting the efficient use of resources, and when appropriate, cost-containment. 1314
Sub-action 1. Carefully consider and align different provider payment methods for PHC
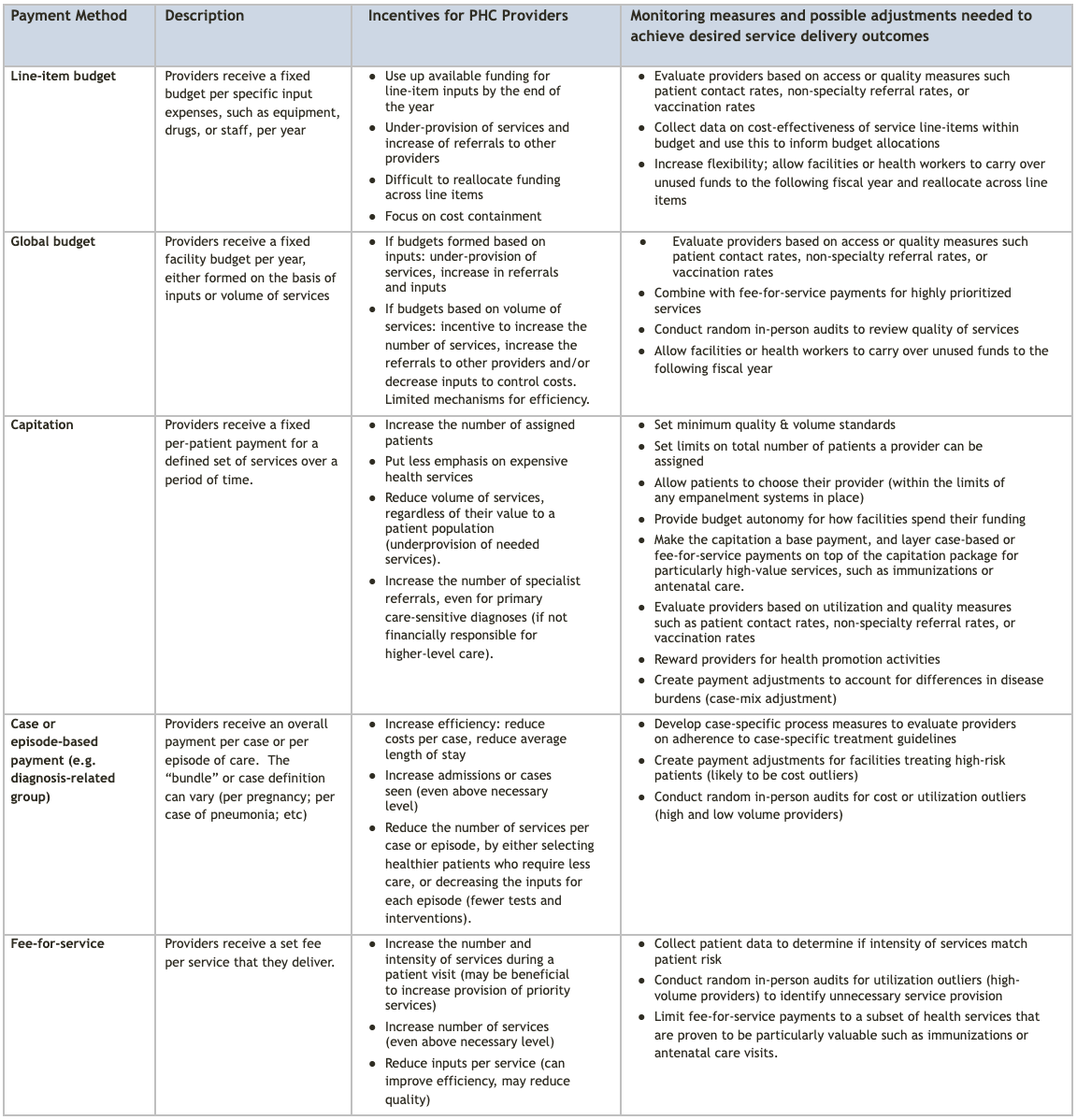
All payment methods have trade-offs, but a carefully designed blend of provider payment methods can incentivize health workers to deliver the right care in the right setting at the right time. Understanding and managing the incentives associated with different provider payment methods is important. 33
Key activities
- Decide on health system objectives: policymakers should review and prioritize the overall objectives for the system, whether they be increased health spending efficiency, cost-containment, improved access, improved quality, administrative simplicity, or a combination of multiple objectives. 34
- Decide on provider payment methods: once health system objectives have been discussed and agreed upon, policymakers should determine which mix of s produces the best set of incentives for providers. 3334 See the table in the purchasing and payment deep dive for a list of common payment methods.
- Ensure adequate balance in expenditure risks: policymakers should aim for a good balance of expenditure risks between purchasers and providers in order to best support high-quality, accessible PHC. 34
- Implement cost-sharing strategies: purchasing agencies can influence provider behaviour and patients’ care-seeking behaviour through payment methods and cost-sharing, helping to achieve a more optimal allocation of resources while ensuring that good quality care is being provided. 13 Cost-sharing requires “that they be kept simple [a fixed amount rather than a percentage] and clear and low– with protection for the most vulnerable”. 35
- All while increasing the capacity of purchasing agencies: Provider payment arrangements that balance purchasers’ and providers’ expenditure risk with the promotion of quality require both effective institutional governance and effective information management systems. In particular, managing a blended payment scheme with different incentives for different services and types of providers is highly complex and data-intensive. Purchasing agencies will likely need strong political support (especially if payment reforms are unpopular with provider groups), investments in a managerial capacity and modern information systems to implement an aligned mix of payment methods.
Sub-action 2. Establish contracts with providers and continuously monitor how different payment methods affect PHC
When it comes to purchasing and payment systems, most if not all payment methods can have unintended consequences. 16Careful monitoring, as well as complementary administrative mechanisms measures, are thus needed to counter undesirable incentives of a given payment method. This also helps to ensure that payments over time continue setting the right incentives to providers. 14
- Monitor service utilization trends: at the community level, these service utilization trends can be used to evaluate whether providers are achieving improved health outcomes for their patients, and payments can be adjusted to reward or incentivize good performance
- Establish contracts with providers: while there is no one-size-fits-all payment model, health system managers should establish contracts with providers that promote high-quality service delivery. For example, offering financial and non-financial incentives for providers to meet targets related to access, equity, and quality of care (see how Costa Rica did this here)
- Use data to measure performance: health systems managers can use data recorded during patient encounters (including data on whether staff are meeting quality standards) to monitor patient outcomes and overall quality of care
- Minimize any kind of incentive that might lead to poor service quality
- Make adjustments if payment arrangements are leading to detrimental effects
- All while ensuring appropriate remuneration: examining the timeliness and predictability of salary payments to health care providers can identify challenges related to low motivation, absenteeism, and/or the presence of informal payments at the primary care level. Delays in payment are often related to weakness in public financial management and/or challenges with cash flow at the central level. Increased advocacy to the Ministry of Finance, coupled with support for overall financial management reforms, is likely to be critical.
Related elements
- Policy & leadership
- Organisation of services
- Adjustment to population health needs
- Funding & allocation of resources
- Population health management
- Management of services
Relevant tools & resources
- Global Health Workforce, 2022: Assorted resources for workforce compensation and incentive strategies
- United Nations, 2022: UN Member States common systems of salaries, allowances, and benefits (including how to calculate staff remuneration rates)
- WHO, 2022: Compendium of resources on promoting strategic purchasing
- WHO, 2021: From value for money to value-based health services: a twenty-first-century shift
- USAID, 2019: Leapfrog to value report
- WHO, 2019: Analytical guide to assess a mixed provider payment system
- Joint Learning Network, 2018: Designing Health Benefits Policies: A Country Assessment Guide
- Joint Learning Network, 2017: Financing and Payment Models for Primary Health Care: Six Lessons from JLN Country Experience
- WHO, 2017: Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. for UHC: key policy issues and questions
- OECD, 2016: Better Ways to Pay for Health Care
- WHO, 2012: Rapid Retention Survey Toolkit: Designing Evidence-Based Incentives Incentives refer to, “a particular form of payment which is intended to achieve some specific change in behaviour. Incentives come in a variety of forms, and can be either monetary or non-monetary.” for Health Workers Health worker retention toolkit
- R4D, 2013: Provider Payment Reform and Information Technology Systems: A Chicken and Egg Question
- R4D, 2009: Making Health Markets Work for the Poor: Improving Provider Performance
- R4D, 2009: Performance Incentives Incentives refer to, “a particular form of payment which is intended to achieve some specific change in behaviour. Incentives come in a variety of forms, and can be either monetary or non-monetary.” in Provider Purchasing and Contracting Arrangements: Rationale and Experiences
- World Bank, 2009: Designing and Implementing Health Care Provider Payment Systems : How-To Manuals
- IntraHealth International, 2000: Health workforce incentive and remuneration strategies
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Understanding and identifying the drivers of health systems performance--referred to here as “related elements”--is an integral part of improvement efforts. We define related elements as the factors in a health system that have the potential to impact, whether positive or negative, the management of services. Explore this section to learn about the different elements in a health system that should be improved or prioritized to maximize the success of actions described in the “take action” section.
While there are many complex factors in a health system that can impact the management of services, some of the major drivers are listed below. To aid in the prioritization process, we group the ‘related elements’ into:
Upstream elements
We define “upstream elements” as the factors in a health system that have the potential to make the biggest impact, whether positive or negative, on purchasing & payment systems.
- Policy & leadership
-
PHC policies and leadership establish financing and expenditure plans and processes. PHC policies should include costed service packages and holistic strategies, including accounting for social determinants of health.
- Adjustment to population health needs
-
Priority setting can help determine how to prioritize purchasing and payment systems to support PHC.
Complementary elements
We define “complementary elements” as the factors in a health system that have the potential to make an impact, whether positive or negative, on the health workforce. However, we consider these drivers as complementary to, but not essential to performance.
- Multi-sectoral approach
-
Social accountability mechanisms can support the monitoring of PHC spending and hold stakeholders accountable for commitments made.
- Population health management
-
Participatory and evidenced-based local priority setting should help to inform how to structure purchasing and payment systems to appropriately allocate limited resources to PHC at the sub-national level.
- Funding & allocation of resources
-
The funding and allocation of resources for PHC can be related to the structures for Purchasing & Payment Systems, however, the direction of influence is circumstantial and often complementary.
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Countries seeking to improve purchasing & payment systems can pursue a wide array of potential improvement pathways. The short case studies below highlight promising and innovative approaches that countries around the world have taken to improve.
PHCPI-authored cases were developed via an examination of the existing literature. Some also feature key learnings from in-country experts.
- East Asia & the Pacific
-
- China, Indonesia, and the Philippines: Case studies on strategic purchasing practices
- China: Health provider payment reforms
- Indonesia: Capitation for primary care with some performance adjustments
- Indonesia: Puskesmas and the Road to Equity and Access
- Thailand: Improving geographic and financial access to care & strengthening primary care in Thailand
- Europe & Central Asia
-
- Armenia: Strategic purchasing for better health
- Estonia: Blended provider payment mechanisms to promote PHC
- Estonia: Establishing family medicine as a specialty to strengthen primary health care
- Kyrgyz Republic: Governance for strategic purchasing in Kyrgyzstan's health financing system
- Mongolia: Assessment of Systems for Paying Health Care Providers in Mongolia: Implications for Equity, Efficiency and Universal Health Coverage
- Multiple countries: Provider payment reforms: lessons from Europe and America for South Eastern Europe
- Romania: Provider Payment Reforms for Improved Primary Health Care in Romania
- Latin America & the Caribbean
-
- Argentina: Strengthening the purchasing function on through results-based financing in a federal setting: lessons from Argentina’s program sumar
- Argentia: Measurement to Ensure Effective Universal Health Coverage: Plan Nacer/Programa SUMAR
- Chile: Measuring Primary Health Care System Performance Using a Shared Monitoring System in Chile
- Costa Rica: Performance measuring and monitoring for continuous quality improvement
- Middle East & North Africa
- North America
- South Asia
- Sub-Saharan Africa
-
- Ethiopia: Strengthening Primary Health Care Systems to Increase Effective Coverage and Improve Outcomes in Ethiopia
- Nigeria: Examining healthcare purchasing arrangements for strategic purchasing in Nigeria: a case study of the Imo state healthcare system
- Rwanda: Effects of performance incentives for community health worker cooperatives
- Sub-Saharan Africa: Strategic Purchasing Africa Resource Centre
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
Building consensus on what strong purchasing & payments systems look like and key strategies to fix gaps is an important step in the improvement process.
Below, we define some of the characteristics of strong purchasing & payment systems in greater detail:
-
Paying for health services can often be a massive burden to patients and their families. works to protect patients and their families from financial hardship and risk. Strategic payment systems can promote the financial protection of patients by:
- Avoiding out-of-pocket payments as a financing source
- Moving towards compulsory pre-payment for health care (including PHC), based on patients' ability to pay
- Using targeted subsidies to ensure access and financial protection for disadvantaged populations
For specifics on how exactly one can promote financial protection, continue on to the “What Actions Can I Take?” section. Below is a deeper dive into the rationale behind why these three methods can work to promote financial protection:
Out-of-pocket payments as a source of financing for health and PHC
To ensure that people can afford PHC, policymakers should avoid relying on out-of-pocket payments. Out-of-pocket payments reduce people’s use of needed services, especially among the poor. When PHC is financed this way, a household’s ability to pay determines whether or not they use health services, and payment is often incurred exactly when the household is most vulnerable – at the time of sickness. Health systems funded on the basis of a large share of out-of-pocket payments tend to be regressive in who makes financial contributions, requiring a larger percentage of income from low-income earners than from high-income earners, as well as inequitable in who uses care and who experiences better health outcomes. 1 There is a large body of evidence concluding that user fees can negatively impact demand for health care contribute to household impoverishment and promote general inequities in health access. 234
While an individual primary care consultation may not be high-cost in absolute terms, out-of-pocket expenditure for primary care services can be prohibitively expensive for many people when the need for care becomes chronic or when medicines are needed (for instance, treatment for TB or routine care for chronic diseases). Spending on basic services can also sometimes be catastrophic (exceeding a substantial share of a household’s income or consumption, like 10% or 25%) or impoverishing (pushing a family below the poverty line or further into poverty). 567
Compulsory prepayment and pooling for health care (including PHC)
means people are asked to make their financial contributions to the health system before they need health care, not when they fall ill. 8 To protect people from financial hardship associated with health care costs, health care contributions should be collected in advance in a predictable manner, unrelated to when health care is needed. Evidence indicates that no country has achieved UHC based on a system organized around voluntary contributions. 9 Voluntary health insurance can provide some financial protection for those (often few) who are covered, but insurers have an incentive to exclude sicker, higher-risk individuals from coverage, and/or charge them higher premiums. As a result, those most in need of health services and financial protection may be unable to afford voluntary health insurance premiums and remain without adequate health coverage. 1 Moreover, voluntary health insurance creates many risks and potential spill-over effects for the rest of the health system, such as shortages of skilled health workers in government facilities and rising prices and costs across the health system. Therefore, “VHI needs to be managed and regulated in such a way that it contributes to equitable progress towards UHC, or at least does not harm such progress”. 10
There are various ways to pool funds and address fragmentation. 911 serves to spread the financial risk associated with the need to use and pay for health services so that this risk is not fully borne by the individual who falls ill.
Targeting to ensure access and financial protection for disadvantaged populations
Various geographic, sociocultural, and economic factors limit access to PHC among poor and vulnerable groups, even if they are eligible “on paper” to have coverage. Targeting (actively identifying) those vulnerable groups and funding their coverage can expand access for those groups.
Significant investments in infrastructure may also be needed to expand coverage to underserved groups. To ensure that targeted free care policies are successful, facilities will likely need increased funding to compensate for the loss of user fees and increased demand for care. New incentives for providing “free” services and efforts to strengthen providers’ capacity to deliver those services are important. 12 In addition, the targeting process has administrative costs; targeting mechanisms require an adequate administrative capacity to be effective and to minimize errors of inclusion or exclusion.
-
Purchasing refers to the transfer of pooled funds on behalf of the covered population to health service providers to deliver health services. means linking the allocation of funds to providers with information on their performance and the health needs of the population that they serve. 8 How countries purchase health care is a critical policy lever that can have a large impact on health system performance, including access to and quality of PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. . A well-aligned mix of s can encourage providers to promote access to necessary health services for patients, incentivize quality of care, and improve equity while promoting the efficient use of resources, and when appropriate, cost-containment. 1314 Ways to utilize strategic purchasing include:
- Consider and align the incentives of different provider payment methods for PHC
- Establish contracts with providers, monitor how different payment methods affect PHC delivery & apply complementary administrative mechanisms
Carefully considering and aligning incentives of different provider payment methods for PHC
Given the diverse set of services required for strong PHC, there is no single best that will work for all services in all settings. All payment methods have trade-offs, but a carefully designed blend of provider payment methods can incentivize health workers to deliver the right care in the right setting at the right time. Understanding and managing the incentives associated with different provider payment methods is important. Patient cost-sharing arrangements are also important influences on patient care-seeking behaviour and also need to be aligned with payment methods and adequately designed. 15 Patients might be unaware of the full cost of the services they are using (and thus possibly use more than they really need), while providers may dispense unnecessary care. Alternatively, providers may not provide enough high-quality care if they are trying to limit their financial outlays.
Establish contracts with providers, continuously monitor how payment methods affect PHC delivery and apply complementary administrative mechanisms
All payment methods can have unintended consequences. 16 Careful monitoring, as well as complementary administrative mechanisms measures, are thus needed to counter undesirable incentives of a given payment method and also to ensure that payments over time continue setting the right incentives to providers. 14
Below is a table of common provider payment methods for PHC that can be mixed and leveraged in order to create a system. For example, capitation payments for PHC. A number of countries have adopted a capitated payment method for PHC services PHC services refer to any intervention, procedure, regimen, or process that providers use to respond to the needs and demands of their patient population at the primary care level. Because of PHC’s community-facing orientation, services can be provided virtually or face-to-face in homes, communities, or PHC centres. Depending on the context, services may be provided by public or private providers. . 17 Capitation minimizes expenditure risk for the purchasing agency because the payment per person for a defined period is set in advance. When paired with patient registration (based on patient choice of their primary care provider or assigning patients to individual primary care providers), 18 and strong quality monitoring systems, capitation can promote efficiency and population health. However, in the absence of patient registration and strong monitoring, capitation can also lead to under-provision and poor quality of essential care, as well as excessive referrals of sick patients to higher-level settings of care. To offset some of the perverse incentives associated with capitation, some countries have had success with blended payment models, such as adding fee-for-service payments for priority services like immunizations or PHC-sensitive communicable diseases. 19
Table 1. Common provider payment methods for PHC 8162021
-
The use of primary care services can often be incentivized through a high remunerations rate. 2223 Remuneration Remuneration is traditionally seen as the total income of an individual that may take different forms, such as salary, stipend, honorarium, and/or monetary incentives. A remuneration strategy determines this particular configuration or bundling of payments that make up an individual’s total income. The World Health Organization recommends that all occupations of the health workforce be remunerated with a financial package in accordance with the employment status and applicable laws and regulations in the jurisdiction. is the payment(s) made to primary care workers for their work or services. It includes the payment of wages and salaries (including benefits and allowances) and consultancy fees, where applicable. Delayed or irregular payments will often have a negative impact on health workers and can lead to demotivation, mistrust, and absenteeism. If health workers do not receive their salaries, they may charge informal payments to patients or refer patients in public facilities to their own private clinics in an effort to make up for lost wages. 24 Over the long term, staff remuneration challenges can make health workers less interested in taking a government-funded health care position in the first place, contributing to staffing shortages in the public sector.
Thus, it is important that funds in a health system are managed in such a way that remuneration of primary care staff happens reliably--regardless of subnational area or facility type. This means that a facility/country’s remuneration method is: 242526
- Stable: the amount paid to staff is consistent in quantity with the amount specified in the working agreement or contract
- Predictable: the timing and delivery mechanism can be anticipated
- Timely: the payment occurs promptly and when specified in the working contract
More information on health workforce incentives and remuneration strategies can be found here.
-
- Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. : Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing Purchasing refers to the transfer of pooled funds on behalf of the population to health service providers to deliver health services. Strategic purchasing means actively linking the allocation of funds to providers with information on their performance and on the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. means actively linking the allocation of funds to providers with information on their performance and the health needs of the population that they serve. It includes decisions on what to buy (including designing benefits policies) from whom to buy, and how to pay (including selecting provider payment methods); as well as establishing the governance and institutional arrangements as well as information management systems necessary for monitoring and managing purchasing arrangements. 114
- Provider payment method Provider payment methods refer to the mechanisms used to transfer funds from a purchaser of health care services to providers. : Provider payment methods refer to the mechanisms used to transfer funds from a purchaser of health care services to providers. 13
- Financial protection Financial protection means that individuals and households do not experience catastrophic or impoverishing expenditure as a consequence of paying for health care. : Financial protection Financial protection means that individuals and households do not experience catastrophic or impoverishing expenditure as a consequence of paying for health care. means that individuals and households do not experience catastrophic or impoverishing expenditure as a consequence of paying for health care. 8
- Earmarking Earmarking means ring-fencing, or protecting, all or a portion of a tax or other revenue source for a particular purpose, such as a specific health program or service. : Earmarking Earmarking means ring-fencing, or protecting, all or a portion of a tax or other revenue source for a particular purpose, such as a specific health program or service. means ring-fencing, or protecting, all or a portion of a tax or other revenue source for a particular purpose, such as a specific health program or service. 27
- Prepayment Prepayment refers to persons or households making payments to the health system before they need health care, not when they fall ill. : Prepayment Prepayment refers to persons or households making payments to the health system before they need health care, not when they fall ill. refers to persons or households making payments to the health system before they need health care, not when they fall ill. 8
- Pooling Pooling is the accumulation and management of financial resources to ensure that the financial risk of having to pay for health care is borne by all members of the pool and not by the individuals who fall ill. The main purpose of pooling is to spread the financial risk associated with the need to use health services. : Pooling Pooling is the accumulation and management of financial resources to ensure that the financial risk of having to pay for health care is borne by all members of the pool and not by the individuals who fall ill. The main purpose of pooling is to spread the financial risk associated with the need to use health services. is the accumulation and management of financial resources to ensure that the financial risk of having to pay for health care is borne by all members of the pool and not by the individuals who fall ill. The main purpose of pooling is to spread the financial risk associated with the need to use health services. 8
PHCPI is a partnership dedicated to transforming the global state of primary health care, beginning with better measurement. While the content in this report represents the position of the partnership as a whole, it does not necessarily reflect the official policy or position of any individual partner organization.
References:
- McIntyre D, Kutzin J. Health financing country diagnostic: a foundation for national strategy development . World Health Organization; 2016.
- Qin VM, Hone T, Millett C, Moreno-Serra R, McPake B, Atun R, et al. The impact of user charges on health outcomes in low-income and middle-income countries: a systematic review. BMJ Glob Health. 2018;3(Suppl 3):e001087.
- Lagarde M, Palmer N. The impact of user fees on health service utilization in low- and middle-income countries: how strong is the evidence? Bull World Health Organ. 2008 Nov;86(11):839–48.
- Newhouse JP. Risk adjustment: where are we now? Inquiry. 1998;35(2):122–31.
- WHO: Tracking Universal Health Coverage: 2017 Global Monitoring Report. World Health Organization and the International Bank for Reconstruction and Development / The World Bank; 2017.
- Xu K, Evans DB, Carrin G, Mylena Aguilar-Rivera A. Designing Health Financing Systems to reduce catastrophic health expenditures. World Health Organization; 2015.
- Ezat Wan Puteh S, Almualm Y. Catastrophic Health Expenditure among Developing Countries. Health Syst Policy Res. 2017;04(01).
- World Health Organization. HEALTH SYSTEMS FINANCING The path to universal coverage. World Health Organization; 2010.
- Kutzin J, Yip W, Cashin C. Alternative financing strategies for universal health coverage. World scientific handbook of global health economics and public policy: volume 1 — the economics of health and health systems. WORLD SCIENTIFIC; 2016. p. 267–309.
- Organization WH, Mathauer I, Kutzin J. Voluntary health insurance: potentials and limits in moving towards UHC. 2018;
- Mathauer I, Torres L, Kutzin J, Jakabc M, Hansond K. Pooling financial resources for universal health coverage: options for reform. Bulletin of the World Health Organization; 2019.
- Mathauer I, Mathivet B, Kutzin J. ‘FREE HEALTH CARE’ POLICIES: OPPORTUNITIES AND RISKS FOR MOVING TOWARDS UHC. World Health Organization; 2017.
- Langenbrunner JC, Cashin C, O’Dougherty S, editors. Designing and Implementing Health Care Provider Payment System. The World Bank; 2009.
- Mathauer I, Dale E, Jowett M, Kutzin J. PURCHASING HEALTH SERVICES FOR UNIVERSAL HEALTH COVERAGE: HOW TO MAKE IT MORE STRATEGIC? . World Health Organization [Internet]. 2019 [cited 2020 Aug 4]; Available from: https://apps.who.int/iris/handle/10665/311387
- Mathauer I, Dkhimi F. Analytical guide to assessing a mixed provider payment system. World Health Organization; 2019.
- Cashin C, Ankhabayar B, Phuong HT, Jamsran G, Nanzad O, Phuong NK, et al. Assessing Health Provider Payment systems. Joint Learning Network for Universal Health Coverage (JLN), [Internet]. 2015 [cited 2020 Aug 4]; Available from: https://www.jointlearningnetwork.org/resources/assessing-health-provider-payment-systems-a-practical-guide-for-countries-w/
- Financing and payment models for primary health care: six lessons from JLN country implementation experience. Joint Learning Network;
- Safety Net Medical Home Initiative,. Empanelment: Establishing patient-provider relationships. Safety Net Medical Home Initiative; 2013.
- OECD. Better ways to pay for health care. OECD Publishing; 2016.
- Vande Maele N, Xu K, Soucat A, Fleisher L, Aranguren M, Wang H. Measuring primary healthcare expenditure in low-income and lower middle-income countries. BMJ Glob Health. 2019 Feb 21;4(1):e001497.
- Ozaltin A, Cashin C. Costing of Health Services for Provider Payment: A Practical Manual Based on Country Costing Challenges, Trade-offs, and Solutions. 2014 p. 93.
- WHO. Transforming Vision into Action: Operational Framework for Primary Health Care. WHO; 2020 Dec.
- Rajan D. Budgeting for health.
- Lindelow M, Kushnarova I, Kaiser K. Measuring corruption in the health sector: what we can learn from public expenditure tracking and service delivery surveys in developing countries. Pluto Press; 2006 Feb.
- PHCPI. Primary Health Care Progression Model Assessment Tool [Internet]. Primary Health Care Progression Model Assessment Tool. 2019. Available from: https://improvingphc.org/sites/default/files/PHC-Progression%20Model%202019-04-04_FINAL.pdf
- Barroy H, Dale E, Sparkes S, Kutzin J, ISSUES C. BUDGET MATTERS FOR HEALTH: KEY FORMULATION AND CLASSIFICATION ISSUES. World Health Organization; 2018.
- Cashin C, Sparkes S, Bloom D. Earmarking for Health From Theory to Practice. World Health Organization; 2017.
- Jowett M, Kutzin J. Raising revenues for health in support of UHC: strategic issues for policymakers. World Health Organization; 2015.
- Roberts MJ, Hsiao W, Reich M. Getting Health Reform Right : A Guide to Improving Performance and Equity. Oxford University Press; 2008.
- Mathauer I, Vinyals Torres L, Kutzin J, Jakab M, Hanson K. Pooling financial resources for universal health coverage: options for reform. Bull World Health Organ. 2020 Feb 1;98(2):132–9.
- Coady D, Grosh M, Hoddinott J. Targeting of transfers in developing countries: a review of lessons and experience. The International Bank for Reconstruction and Development / THE WORLD BANK; 2004.
- WHO.Budget transfers to health coverage schemes [Internet]. [cited 2019 Dec 20]. Available from: https://www.who.int/health_financing/topics/budget-transfers/en/
- Mathauer I, Dkhimi F. Analytical guide to assess a mixed provider payment system. World Health Organization; 2019.
- Designing Health Benefits Policies: A Country Assessment Guide | Joint Learning Network [Internet]. [cited 2022 Aug 1]. Available from: https://www.jointlearningnetwork.org/resources/designing-health-benefits-policies-a-country-assessment-guide/
- WHO. Primary Health Care on the Road to Universal Health Coverage: 2019 Global Monitoring Report. WHO; 2019.
